Traveling, At Times Can Be Damaging To Your Body!
- By Dr. Anthony Orlando, DPT.
- •
- 18 Jul, 2017

An estimated 222 million people are expected to fly on U.S. carriers this summer season, and if you're one of them, you might not be looking forward to the gross feeling air travel often leaves you with. Besides the airport crowds and stress, traveling at such a high altitude has real effects on the body. One study from the U.K. showed passengers' oxygen levels dropped 4 percent, which could be a concern if you have heart or lung problems. To help prevent headaches, drink plenty of water, and avoid alcohol and caffeine.

Traveling long distances in cars, buses, and planes over the summer could put you at risk for deep vein thrombosis (DVT) -- potentially deadly blood clots in the deep veins of the lower legs and thighs, an expert says.
Sitting for long periods of time in cramped spaces can limit circulation in the legs, resulting in the formation of a blood
clot. The clot can travel through the blood stream and lodge in the lungs, brain, heart and other areas. This can lead to severe damage to organs and possibly death.
However, it's easy to prevent deep vein thrombosis. If you plan to travel overseas or cross country, make sure you get up and walk around at least every two hours, and try not to sleep more than four hours at a time. Drink plenty of water or juices, wear loose-fitting clothing, eat light meals and limit alcohol consumption. Elderly and those with circulation problems should wear compression stockings that help prevent clots from forming in the deep veins.
About 2 million Americans develop deep vein thrombosis every year, and nearly 200,000 die. "It's a very serious condition that can simply be avoided by getting up and moving around," experts say.
"Symptoms include pain and tenderness, swelling, redness and increased warmth in one leg. In some cases, a physician might suggest that a patient go on blood thinners or simply take an aspirin before and during a long trip to avoid [deep vein thrombosis]."
Sitting in tight quarters for hours and hours can affect blood flow throughout your body, leading to swelling in your feet and ankles. It's also well-established that the risk of a blood clot (DVT) increases when blood isn't circulating well, as happens during plane travel. In that position, the veins in our legs are compressed and the blood flow through them is slowed down Although you often hear the advice to get up and walk around, it can cause traffic jams if too many people do it at once, and can be dangerous in the case of unexpected turbulence. Average travelers without any of risk factors would benefit from simple movements of the ankle—rotation, flexion, extension—which can be done in their own seat as frequently as possible. Risk factors for DVT include being obese, pregnant or postpartum, on birth control pills, over age 40, or having a serious medical illness. People with underlying risk factors for DVT benefit from compression stockings, and for some at high risk, even the use of anti-coagulant drugs may be indicated. Talk to your doctor if you have one or more risk factors and are planning a flight this summer. Pay attention to these silent signs of deep vein thrombosis.
DVT Prevention Tips

If you can't get up and move around every couple of hours, Here are few exercises to do while sitting down:
1. Ankle turns: Lift your feet off the floor and move your toes in a circle, one foot moving clockwise and the other foot moving counterclockwise. Change direction and repeat.
2.& 3. Foot lifts: Place your heels on the floor and bring your toes up as high as you can. Then put both feet back flat on the floor. Then pull your heels up while keeping the balls of your feet on the floor.
4. Leg Stretch: Stretch out your legs and point your toes.
5. Knee lifts: While keeping your knee bent, raise your leg while tensing your thigh muscle. Repeat 20 to 30 times, alternating legs.
6. Shoulder rolls: Raise your shoulders and then move them forward, downward and then backward in a smooth circular movement
7. Neck roll: Relax your shoulders, let your head drop to your right shoulder and roll your head slowly to the front and then to your left side. Repeat five times.
8. Walk: When on a bus or a plane walk up and down the isle for a stretch. Be courteous of others and cautious of road bumps and turbulence.
9. Arm bends: Start with your elbows on the armrests and your hands pointed forward so that your lower and upper arms make a 90-degree angle. Take turns moving your left and then your right hand toward your chest and back, and continue for 30 seconds.
10. Knee to chest: Bend slightly forward. Fold your hands together around your left knee and pull it toward your chest. Hold this position for 15 seconds and let your knee drop slowly. Change legs and repeat.
11. Forward bends: Place both feet on the floor and pull your abdomen in. Bend slowly forward and ''walk'' your fingers along your shins to your ankles. Hold for 15 seconds and sit up slowly.
12. Upper-body stretch: Stretch both arms over your head. With your right hand, grab your left wrist and pull it slowly to the right. Hold for 15 seconds and change arms.
13. Shoulder stretch: With your right hand, grab your left elbow and pull your outstretched left arm slowly toward your right shoulder. Hold for 15 seconds and change arms.
Stay active during long distance travels to prevent blood clotting and DVT.
References
What Traveling on a Plane Does to Your Body. Tina Donvito
Lengthy Car, Plane Ride Pose Risk of Clots. 11/23/13, Healthy Day.
infographic Image Source: Stay Sure.
Additional Articles

Temporomandibular joint disorder (TMD) is a common condition that limits the natural function of the jaw, such as opening the mouth and chewing, and can cause pain. The temporomandibular joint (TMJ) is a hinge joint that connects your jaw to your skull in front of your ear. The TMJ guides jaw movement and allows you to open and close your mouth and move it from side to side to talk, yawn, or chew.
Symptoms of TMJ include Jaw pain or Jaw fatigue, Difficulty opening your mouth to eat or talk, Ringing in your ears, Dizziness, Headache, Popping sounds in your jaw, Neck pain, Locking jaw.

Aquatic Therapy is defined as physical therapy that takes place in a pool or another aquatic environment under the supervision of a trained healthcare professional. Aquatic therapy is also known as water therapy, aquatic rehabilitation, pool therapy, therapeutic aquatic exercise or hydrotherapy.
Common goals of aqua therapy programs include: Improving flexibility, balance and coordination.Building muscle strength and endurance. Enhancing aerobic capacity, Assisting with gait and locomotion. Lastly, reducing stress and promoting relaxation
It is different from aquatic exercise or aquatic fitness because it is a physical medicine and rehabilitation specialty that requires the involvement of a trained professional and is covered by many insurance providers due to the personalized nature of the treatment.
Aquatic therapy should not be confused with adaptive aquatics, either. Adaptive aquatics is the process of teaching people with disabilities how to swim safely in the water. Aquatic therapy does not focus on teaching clients how to swim.
There are different types of aquatic therapy, listed below are a few popular examples.
- Hydro-Massage a relaxing form of water-based hydrotherapy massage that can take place in a dedicated spa pool or in a specially designed bath.
- Aqua Running provides an excellent cardiovascular workout, but can lead to joint damage. However, with an underwater treadmill, it’s possible to enjoy all the benefits of running.Underwater treadmills can be used to help athletes recover from injuries or to regain full-body motion after surgery.
- Bad Ragaz Ring Method's goal is to develop a water-based strengthening and mobilizing resistive exercise model through the use of combined elements of aquatic exercise techniques. The “ring” portion of the name of this water therapy technique refers to the ring-shaped flotation devices used to support the client as they move across the water’s surface.
- Burdenko Method is often used for treating sports-related injuries. It works to improve a patient’s speed, strength, flexibility, coordination, balance and endurance by performing rehabilitative exercises in the water and progressing into performing the exercises on land as their condition improves.
- Halliwick Concept focuses on helping clients develop balance and core stability.

The weather is warming up and that means people are out, about and doing more. For many people that means summertime sports, vacation, golf, running and even rigorous gardening and lawn chores. These activities are great to engage in but be aware that they can lead to a wide range of injuries such as runner's knee, tennis elbow, back pain and strain, tendinitis and more. When these things happen it is recommended to see either a physical therapist or a doctor to not only get fast relief, but also to address the underlying issues causing pain.
When sports injuries occur it is important to get the right kind of help. It is one thing to treat or manage the pain, which is what traditional medicine offers. This is generally done through treatment with pain medications or anti-inflammatory treatments but doesn't address the root cause of the injury at all. Physical Therapy provides a natural alternative for treatments and addresses the cause of pain while simultaneously providing some degree of relief for the pain almost immediately.
Educators have the opportunity to make a huge impact on their students – however, they face many challenges, which may result in low back, neck and shoulder pain; tired feet, aching legs, headaches, insomnia and stress. Often, the number one concern for teachers is back pain when standing.
Whether you’re a nursery school teacher or a college professor, job-related challenges can be reduced or avoided, especially if you know how to improve posture. Challenges include: teachers often stand “lecture-style” for extended hours, placing an extra burden on the low back and legs, which may lead to poor posture. Additionally, hard unforgiving surfaces can take their toll after prolonged standing. Bending or stooping over children at their desks and sitting down for long periods when grading assignments.

Patellofemoral pain syndrome (PFPS), or runner's knee, got its nickname for an obvious and very unfortunate reason—it's common among runners. The stress of running can cause irritation where the kneecap (patella) rests on the thighbone. The resulting pain can be sharp and sudden or dull and chronic, and it may disappear while you're running, only to return again afterward. While biomechanical issues may be to blame for runner's knee, the cause can often be traced back to poorly conditioned quadriceps and tight hamstrings.
Weak quads aren't able to support the patella, leading it to track out of alignment, and inflexible hamstrings can put pressure on the knee. If you want to treat and avoid another bout with runner's knee, add strengthening and stretching to your routine.


What did you learn growing up that you implement in your physical therapy practice now?
Compassion and empathy to go along with the knowledge. I think that’s all people want from anybody. Just be honest, be a little compassionate with me. Especially people who are in pain. They don’t want to come through the door complaining. They’re hurting. You’re an outlet for them.
How do you get started with a new patient?
The first thing I ask is, “How can I help you?” Because you’re here and I’m here to help you. It’s not my therapy.
What happens once you’re working with patients who say they’re starting to feel better from the treatment?
Hopefully they’re saying, “I’m a lot better.” I’ll go through what I just did with them and then I’ll try to incorporate exercises. Now at this point I’m trying to empower you as the patient. It’s not about me now. I always give exercises that you’ll be able to do in a timely fashion.
What happens once a patient is empowered in your care?
It’s about you talking about your problems and me, like a scientist, I’m just helping you interpret those results. We’re working as a team. And that empowers people, too. They feel like they’re part of this.
If you sense patients are stressed in their everyday lives, what can you do for them?
I tell people, “Put your phone over there. Forget about the phone. You’re a slave to your phone.” So they’ll put the phone away. I have dim lighting. I have the aromatherapy in my room. And I have Pandora so they can pick the music. That’s it. I’ll leave them in there for 15 to 20 minutes. In that time, they get to integrate all this. It lets them unwind. They get to decompress. They get to unplug. And they get to appreciate the whole therapy. I’ve incorporated not only therapy, but the experience. Usually people will come out and say, “I feel great.” After a while I’ll get people saying, “I couldn’t wait to get here.” When do you hear people say they couldn’t wait to get to a medical office?
What is the best exercise?
I get that question a lot. I’ll throw it right back at them -- “What do you think is the best exercise?” They all say the same thing. “Well, walking, right?” I say, “Maybe.” They’ll say, “What about swimming?” I’ll say, “You know what? Those are two good exercises, but it’s a trick question. The best exercise is the one you’ll do.”
What if patients say their doctor has told them to stop working out? Can you still recommend exercises?
Let’s work on the problem. If something you do is part of who you are and you feel good about that, then I just want to support that. But I want to support it in a safe way so you don’t get injured. That’s where I’ll come in. Because I really understand that injury has a psychological and a spiritual effect. You start to lose your focus on things because you don’t feel good about yourself. So I’ll constantly support you in what you do; I’ll just modify certain things. You still have who you are, but you’re doing it in the safest way possible.

A) To help bio mechanical abnormalities related to pain.
e.g. flat feet
B) To help accelerate tissue repair by temporarily supporting and uploading injured soft-tissues
e.g. Rotator Cuff tendonitis / partial tear
C) To help temporarily support hyper-mobile segments or joints
e.g. Sacro-iliac joint (SIJ) hyper-mobility and pain (very common in pregnant women)
D) To help unload stress and reduce pain from hyper tonic / overactive muscles
e.g. Muscle Tension in the Neck and Low back
E) To help restrict and limit potentially aggravating postures and movements
e.g. Lumbar flexion and rotation for low back pain
F) To help facilitate muscle activity, in order to increase the effectiveness of therapeutic exercises
e.g. Knee pain from poor tracking of the kneecap (very common in runners)
G) To help relieve acute perfuse myofascial pain
e.g. Whiplash Associated Disorders
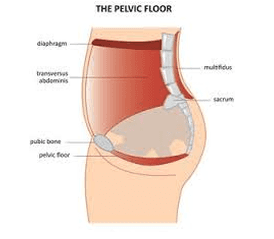
The cause of Pelvic Floor Dysfunction is often caused by pregnancy, trauma from a car accident, infections, or surgery. Sometimes a gym injury can bring it on. Even doing too many kegels or rough menstrual cramps can cause PFD to manifest itself.
Symptoms of PFD range from a muscle or groin pull, frequent or painful urination, lower back pain, constipation or painful intercourse, yet the diagnosis is sometimes hard to get. When you are in pain in the pelvic or groin region, doctors will test for infections and come up empty. Often PFD is the cause. If not treated properly, PDF can go on to affect the bladder causing incontinence, IBS or Irritable Bowel Syndrome, certain sexual dysfunctions, trouble sitting for long periods and other related pain.
Yet all is not lost. Physical Therapy has been known to have excellent results ranging from relief to full recovery. Some of the options available for patients of PFD include trigger point release massage, connective tissue manipulation, heat and cold therapy, electrical stimulation, deep tissue massage, mysofascial release, biofeedback, ultrasound, and rehab including strengthening exercises and Pilates
These exercise can range from simple pelvic tilts while lying on the floor, to lying on a tennis ball to release the tension and re-educate the muscles around the sacroilliac joint, to simple Pilates moves, like sit ups and stretches, to strengthen the entire core and the pelvic floor.
With a well-rounded physical therapy program in place, patients will heal and achieve a better level of health and fitness overall.


